肝脏黄素单加氧酶(flavin-containing monooxy genases, FMOs, E.C.1.14.13.8) 是机体参与治疗药物或外源物生物转化的Ⅰ相代谢酶, 其重要性仅次于CYPs。FMOs属于B类黄素蛋白单加氧酶家族, 即依赖黄素腺嘌呤二核苷酸(flavin adenine dinucleotide, FAD)、还原型烟酰胺腺嘌呤二核苷酸磷酸(nicoti namide adenine dinucleotide phosphate oxidase, NADPH)和分子氧、且不含亚铁血红素的单加氧酶[1]。在新药研发过程中, 设计由FMOs参与代谢的候选药物具有以下优势: ① FMOs可催化的底物广泛:基于其特殊的蛋白结构和催化机制, FMOs几乎可以氧化所有软亲核、高极性含氮、硫的杂原子化合物, 也可催化某些碳原子氧化, 如氧化脱氟以及酮或醛的Baeyer-Villiger反应生成酯[2, 3]; ② FMOs能将化合物转变成高极性、低毒且易于排泄的代谢产物, 不易发生代谢产物蓄积; ③ FMOs不易被诱导或者抑制, 可以降低药物-药物相互作用带来的不良反应; ④ FMOs与人体某些疾病和生命过程有关。因此, FMOs在药物代谢、新药研发以及新药靶点发现中的作用日益受到重视。
1 FMOs的发现与命名以往研究曾认为, CYP450可催化亲核杂原子化合物的N-氧化或S-氧化。直到20世纪70年代, Ziegler等[4]在猪肝微粒体中纯化出一种可催化胺类药物N-氧化的混合功能氧化酶。分子质量和黄素蛋白含量均高于CYP450, 催化过程依赖NADPH和O2, 不受细胞色素的影响, 且对一氧化碳不敏感, 自此确认该酶为黄素单加氧酶FMOs。80年代初期, Tynes等[5]将大鼠、小鼠和兔子的肝、肺和肾FMOs与纯化猪肝微粒体FMOs进行比较, 发现上述不同种属组织中的FMOs具有相似的催化能力, 但兔肺中FMOs的形态和底物特征与肝脏不同, 随后证明其与肝微粒体FMOs是不同的亚型。90年代末, 研究者克隆并纯化出不同组织和不同种属的FMOs蛋白。目前已鉴定出FMO基因有11种(FMO1p~FMO11p), 其中只有FMO1p~FMO5p能编码具有催化功能的蛋白, 其序列相似性为52%~60%, 分别命名为FMO1~FMO5[6]。
2 FMOs的生物学特征2.1 FMOs的蛋白结构FMOs蛋白的分子质量约为60 kDa, 其532~ 558个氨基酸残基中包含高度保守的黄素腺嘌呤二核苷酸-(flavin adenine dinucleotide, FAD)和NADPH-结合结构域。FMOs晶型结构包含一大一小两个结构域。在大结构域的下半部分包含FMOs识别序列FXGXXXHXXXF, 能与FAD的异咯嗪环相互作用; NADPH的腺嘌呤与小结构域结合, 以烟酰胺基团与FAD的异咯嗪环重叠形成氢键[7]。
2.2 FMOs的含量测定以往FMOs相对含量测定通常应用蛋白免疫印迹法(Western blots)或以FAD的浓度来预测FMOs的绝对含量, 但这种方法测定的是全蛋白, 而非FMOs总蛋白含量(总蛋白=全蛋白+脱辅基蛋白)[8], 存在一定局限性。目前以UPLC-MRM为基础的靶向定量蛋白质组学方法已经广泛应用于人肝微粒体FMOs蛋白测定[9]。
2.3 FMOs活性测定的影响因素以FMOs特异性底物苄达明的氮氧化为活性检测指标, 考察不同实验条件对人肝微粒体FMOs活性影响发现, 45 ℃预温孵5 min可使FMOs活性降低70%; DMSO (0.1%和0.5%)可剂量依赖地抑制FMOs活性, 而甲醇(0.5%)和乙腈(0.5%)影响较小; 肝微粒体在缺乏NADPH的条件下37 ℃预温孵5~10 min, FMOs活性降低30%~50%; FMOs活性在pH 8.4时高于pH 7.4;竞争性抑制剂甲硫咪唑能显著抑制FMOs活性等[10]。
3 FMOs的催化机制FMOs需要以FAD为辅基、NADPH为辅助因子、分子氧为共底物完成催化过程。首先, 辅助因子NADPH结合FAD, 并将其迅速还原成FADH2。接受了两个电子的还原形FAD迅速与分子氧结合, 形成稳定的C4位黄素过氧化中间体, 等待与适当的亲核底物RSH结合[11]。通过底物对FADH-OOH的亲核攻击, 一个氧原子转移到底物上, 形成氧化产物(RSOH), 另一个氧原子形成水, 从而使FADH-OH还原为FAD, 并释放出NADP+等待下一轮催化循环(图 1)[12]。因FMOs在催化过程中并没有形成经典的酶-底物复合物, 因此Km主要反映底物与酶活性位点接近的难易程度, 而底物的大小和形状以及化合价是决定其能否与酶活性位点结合的关键因素[13]。
 |
Figure 1 Catalytic mechanism of flavin-containing monooxy genases (FMOs) |
与CYPs的催化机制不同, FMOs不需要还原酶就可直接被NADPH还原, 并在不结合底物的情况下直接活化氧分子, 形成稳定的中间体, 氧化所有能与活性中间体结合的亲核底物, 这一特性提示FMOs底物的广泛性[14]。
4 FMOs的特异性与药物代谢4.1 FMOs的表达差异性FMOs的表达水平存在明显的组织、年龄、性别以及种属差异(表 1)[15-19]。如① 组织特异性:以人为例, 成人肝脏中以FMO3和FMO5为主, 肾和肠中以FMO1为主, 肺中以FMO2为主; ② 发育因素:人胎肝中以FMO1为主, 出生后FMO1表达被抑制, 逐渐以FMO3为主; ③ 性别差异:雄性小鼠肝脏以FMO1为主, 而雌性小鼠肝脏以FMO3为主, 而人FMOs无明显性别差异; ④ 种属差异:与成人肝脏中FMO1低表达不同, 大鼠、小鼠、犬肝中FMO1是主要表达形式, 但雌性小鼠肝脏主要表达FMO3[20]。有研究表明, 食蟹猴体内FMO1~FMO5的表达水平与人的相似性达94%~98%, 且食蟹猴FMO1主要存在于肾脏, FMO3主要存在于肝脏, 因此在研究FMOs介导的药物代谢时, 食蟹猴相对于其他种属而言是较为理想的动物模型[21]。
| Species | Type | Tissue | Age | Gender | Reference |
| Human | FMO1 | The main subtype of adult kidney | Fetal liver expression was high, the expression was silent after birth | No significant gender difference | 15 |
| FMO2 | The main subtype of adult lung | ||||
| FMO3 | The main subtype of adult liver | Fetal liver expression was low and the expression increased gradually after birth | |||
| FMO4 | Pancreas | ||||
| FMO5 | Liver, stomach, pancreas, small intestine | ||||
| Mouse | FMO1 | Lung, kidney | Fetal liver expression gradually increased and reached adult levels after birth | Sex differences occurred 28 days after birth, and the expression of female mice remained unchanged, the expression of male mice was inhibited | 16 |
| FMO2 | Lung | No significant gender difference | |||
| FMO3 | The main subtype of adult female mouse liver | Fetal liver expression was low and reached adult levels 14 days after birth | There were obvious gender differences at 42 days after birth, and adult male mouse could hardly be detected | ||
| FMO4 | Low expression | No significant gender difference | |||
| FMO5 | Liver, kidney, intestine | Fetal liver expression was low and reached adult levels two days after birth | In the liver and kidney, the female mouse was higher than the male | ||
| Rat | FMO1 | Liver | There were obvious gender differences, and male rat was higher than female | 17 | |
| FMO2 | Kidney | No significant gender difference | |||
| FMO3 | Liver (low than FMO1) | ||||
| FMO4 | Low expression | ||||
| FMO5 | Liver | ||||
| Monkey | FMO1 | Kidney | No significant gender difference | 18 | |
| FMO2 | Lung, heart | ||||
| FMO3 | Liver | Fetal liver expression was low and increased gradually after birth | |||
| FMO4 | Kidney | ||||
| FMO5 | Liver, jejunum | ||||
| Rabbit | FMO1 | Liver, intestinal mucosa | No significant gender difference | 19 | |
| FMO2 | Lung | The high expression of fetal lung was inhibited immediately after birth and elevated 21 days later | |||
| FMO3 | Liver (low than FMO1) | ||||
| FMO4 | Low expression | ||||
| FMO5 | Liver |
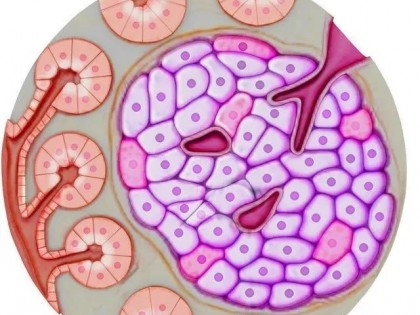
在所有FMOs亚型中, FMO1底物范围最广, FMO3次之。FMO1和FMO3具有部分底物重叠性, 如共同底物苄达明、伊托必利、脱乙酰基甲酮康唑、伏立康唑和他莫昔芬等, 但也有各自选择性底物, 如FMO1可催化氯丙嗪、丙咪嗪和夸西泮, 而FMO3可催化普鲁卡因胺。FMO2底物范围相对有限, FMO4的C-端比其他FMOs多出23~26个氨基酸, 目前未发现FMO4的底物, 且因FMO4表达水平较低, 因此其在药物代谢中的作用暂被忽略[22]。FMO5对经典FMOs底物常表现出较低的催化活性, 目前已知经FMO5催化的含氮、硫化合物较少, 通常认为FMO5在药物代谢中的作用较小。近期证实人FMO5属于Baeyer-Villiger加单氧酶(图 2), 能催化部分碳原子的氧化, 通过在临近羰基(醛或酮)的碳-碳键插入氧原子形成酯, 如抗癌化合物E7016和抗菌药MRX-1[2]。
 |
Figure 2 The Baeyer-Villiger reaction of human FMO5 |
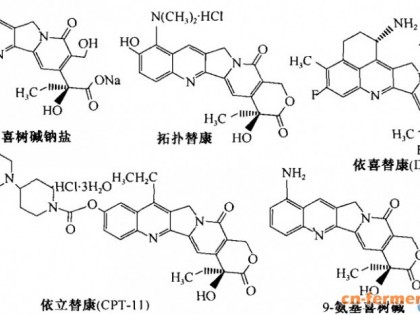
由人FMO1、FMO2、FMO3和FMO5参与代谢的大部分药物为叔胺类或硫化物, 经过氮氧化生成氮氧化物或者经过硫氧化生成亚砜。其次包含伯胺类(如安非他明, 经FMO催化生成N-羟胺, 二次氧化丢掉水生成肟)、仲胺类(如N-脱乙酰甲酮康唑, 先生成N-羟胺, 二次氧化生成硝酮)、硫脲类(如乙硫异烟胺, 经硫氧化生成亚砜)。氮氧化物和硫氧化物是极性较大且易排出体外, 因此由FMOs参与代谢的反应多为解毒过程。由于电荷限制, 内源性化合物很难接近FMOs的活性位点, 但人FMO3能催化酪胺合苯乙胺的氮氧化以及蛋氨酸的硫氧化[23]。部分由人FMO1、FMO2、FMO3和FMO5参与代谢的临床治疗药物见表 2[14, 20, 22-54]。
| Type | Reaction | Substrate | Type of drug | Reference |
| FMO1 | N-Oxygenation | Benzydamine | Nonsteroidal anti-inflammatory | 24 |
| Imipramine | Antidepressant | 25 | ||
| Itopride | Antiemetics | 25 | ||
| Nomifensine | Antidepressant | 25 | ||
| Olopatadine | Antiallergic agent | 26 | ||
| Strychnine | Hypotensor | 27 | ||
| Procainamide | Type Ⅰ antiarrhythmic agent | 22 | ||
| Tamoxifen | Antiestrogen | 28 | ||
| Tazarotenic acid | Retinoic acid receptor modulator | 29 | ||
| Voriconazole | Antifungal agents | 30 | ||
| Xanomeline | M1 receptor agonist | 31 | ||
| Deprenyl | Monoamine oxidase type B inhibitor | 32 | ||
| Lorcaserin | Selective human 5-hydroxytryptamine 2C agonist | 33 | ||
| Methamphetamine | Psychostimulant | 34 | ||
| C-1311 | Antitumor agent | 35 | ||
| GSK5182 | Antidiabetic | 36 | ||
| MK-0457 | Aurora kinase inhibitor | 37 | ||
| S-Oxygenation | Methimazole | Thyroperoxidase inhibitor | 38 | |
| Sulindac | Nonsteroidal anti-inflammatory | 39 | ||
| Sulindac sulfide | Nonsteroidal anti-inflammatory | 40 | ||
| Cimetidine | Antiulcerative | 14 | ||
| Ethionamide | Antituberculosis drugs | |||
| Quazepam | Sedatives and hypnotics | |||
| Selenomethionine | Anticancer drug | 41 | ||
| Thiosemicarbazide | Antituberculosis drugs | |||
| S-Methyl N, N-diethyldithiocarbamate | Antialcoholic | |||
| FMO2 | S-Oxygenation | Methimazole | Thyroperoxidase inhibitor | 14 |
| Ethionamide | Antituberculosis drugs | 42 | ||
| Thiosemicarbazide | Antituberculosis drugs | 43 | ||
| FMO3 | N-Oxygenation | Benzydamine | Nonsteroidal anti-inflammatory | 38 |
| Clozapine | Antipsychotic drugs | 40 | ||
| Olanzapine | Antipsychotic drugs | 41 | ||
| Olopatadine | Antiallergic agent | 44 | ||
| Procainamide | Type Ⅰ antiarrhythmic agent | 42 | ||
| Itopride | Antiemetics | 45 | ||
| Amphetamine | Antipsychotic drugs | |||
| Almotriptan | Antimigraine | 46 | ||
| Dasatinib | BCR-ABL and SRC family kinase inhibitor | |||
| Deprenyl | Monoamine oxidase type B inhibitor | 47 | ||
| Loxapine | Tricyclic antipsychotic | |||
| Nicotine | Analeptic | |||
| Nomifensine | Antidepressant | |||
| Pargyline | Hypotensor | 48 | ||
| Pyrazoloacridine | Anticancer drug | |||
| Furosemide | Anti ulcer drug | |||
| Tamoxifen | Anti estrogen drugs | |||
| Stelazine | Antipsychotic | 20 | ||
| Voriconazole | Antifungal agents | |||
| Xanomeline | M1 receptor agonist | |||
| N-Deacetyl ketoconazole | Antifungal | |||
| Methamphetamine | Psychostimulant | |||
| Moclobemide | Monoamine oxidase type A inhibitor | |||
| N, N-Diallyltryptamine | Pschychostimulant | |||
| TG100435 | Src kinase inhibitor | |||
| MK-0457 | Aurora kinase inhibitor | 49 | ||
| C-1311 | Antitumor agent | 50 | ||
| GSK5182 | Antidiabetic | |||
| K11777 | Peptidomimetic | 51 | ||
| L-775, 606 | 5-HT(1D) receptor agonist | |||
| S-Oxygenation | Methimazole | Thyroperoxidase inhibitor | 35 | |
| Sulindac sulfide | Nonsteroidal anti-inflammatory | 37 | ||
| Thiosemicarbazide | Antituberculosis drugs | |||
| Ranitidine | Anti-ulcer agent | 45 | ||
| Ethionamide | Antituberculosis drugs | |||
| Albendazole | Anthelmintic | 51 | ||
| Altramet | Histamine H2-receptor antagonis | 52 | ||
| Esonarimod | Immunomodulator | |||
| Selenomethionine | Anticancer drug | |||
| Tazarotene | Retinoic acid receptor modulator | 31 | ||
| FMO5 | N-Oxygenation | Nomifensine | Antidepressant | 53 |
| S-Oxygenation | S-Methyl esonarimod | Cytokine production inhibitor | 50 | |
| Phospho-sulindac | Nonsteroidal anti-inflammatory | |||
| Baeyer-Villiger Reaction | E7016 | Anticancer drug | 23 | |
| MRX-1314 | Antibacterials | 54 |
通常情况下FMOs不易被外来物所诱导或抑制, FMOs个体间的数量和活性差异多源自基因变异而非环境因素, 因此研究FMOs的遗传药理学有助于预测药物代谢的个体间差异。真核细胞的FMOs位于内质网膜, 已知FMOs基因家族存在相似的内含子/外显子结构, 说明其来源于同一个祖先基因或一系列基因的复制[55]。人FMOs基因聚集在染色体1上, 人FMO1p到FMO4p和假基因FMO6p聚集在染色体1的1q24.3位, FMO5p在1q21.1位, 假基因FMO7p~FMO11p则出现在1q24.2位。在已经鉴定出来的11种基因型中, FMO1~5具有催化功能, FMO1、FMO3和FMO5是公认参与药物代谢的主要酶, FMOs的基因突变会影响其对药物代谢的作用[56]。
4.3.1 FMO1人体内FMO1主要存于胎儿肝脏、成人肾、肠黏膜和支气管中。胎儿肝脏中FMO1在8~15周时含量最高, 但分娩后FMO3的表达会抑制FMO1, 因此FMO1不是成人肝脏代谢的主要酶[57]。FMO1的遗传变异不明显, 只存在少量编码区的单核苷酸多态性, 突变频率低且对催化活性影响不大。
与其他同工酶相比, FMO1有较大的底物入口通道, 可以选择性氧化三环类抗精神病药丙咪嗪、抗组胺药异丙嗪、溴非尼腊明等[12]。FMO1主要参与含硫化合物氧化, 能将硫酮类底物催化生成次磺酸和磺酸, 并很快分解成咪唑和HCO3-, 因此人肠道和肾脏FMO1的代谢能力和活性可能会影响硫酮类化合物的生物利用度, 甚至导致肾毒性。同时FMO1也参与内源性物质代谢, 起调节体内能量平衡的作用[58]。虽然FMO1在成人的肾脏和肠道中大量存在, 超过了肾脏中CYPs的总量甚至与肝脏中的CYP3A4相近, 但整体来看人肾脏的代谢能力小于肝脏的1/14, 因此FMO1在化合物代谢中的作用并没有预想的大。
4.3.2 FMO2FMO2主要存于大多数哺乳动物的肺组织, 且具有基因多态性。白种人和亚洲人FMO2的基因突变最终翻译成无功能的FMO2 (FMO2*2A), 由于错误折叠或者快速降解使肺组织的FMO2不易测定。非洲(49%以上)和西班牙(2%~7%)人肺中至少有一种FMO2等位基因突变(FMO2*1), 可以编码全长的多肽链, 翻译出有活性的FMO2蛋白[59]。
FMO2具有限定的底物通道和严格的底物选择, 相对于含氮化合物, FMO2更偏向于氧化含硫底物, 如有机磷酸酯杀虫剂甲拌磷。在大多数情况下, 由FMOs参与的代谢会产生低毒产物, 但硫脲或者硫酮类除外。FMO2参与硫脲类在体内的硫氧化, 初始氧化产物是亲电子的次磺酸, 能与亲核物质如谷胱甘肽反应, 并且消耗NADPH, 导致氧化应激或组织损伤。如果次磺酸在体内停留时间过长, 可被FMOs继续氧化, 生成亚磺酸[60]。亚磺酸的反应活性高于次磺酸, 因此会直接损伤细胞或者转化成其他产物。
4.3.3 FMO3FMO3主要存于成人肝脏, 是成人肝脏中发挥主要催化功能的FMOs。分娩过程或产生的未知信号可抑制FMO1表达, 使FMO3表达水平高于FMO1, 在青少年早期达到成人水平[61]。
人FMO3具有明显的基因多态性, 目前已鉴定出多达15种SNPs, 除N61K (酶活性降低)、L360P (酶活性升高)、R205C (舒林酸氧化被抑制)外大部分突变型基本不影响FMOs的活性, 其中V257M、E158K和E308G突变型最为常见[62]。在欧洲和亚洲人中最常见的SNPs是E158K和E308G, 两种SNPs互为关联, 出现在相同的染色体上。(E158K/E308G)变异体使酶活性降低, 如减少体内抗溃疡药甲胺呋硫的N-氧化物的生成, 表现出中等或者短暂的三甲胺尿症的症状[63]。FMO3活性降低也可能是有利的, 如FMO3的突变型影响非甾体抗炎药舒林酸对患有家族性腺瘤性息肉病(familial adenomatous polyposis, FAP)的临床治疗效果。舒林酸是一种前体药物, 在体内由肠道菌群代谢成有效形式―硫化舒林酸, FMO3会将其氧化成非活性产物, 而在E158K和E308G变异体中, FMO3活性降低使硫化舒林酸的氧化程度降低, 从而提高了药物治疗效果[64]。
4.3.4 FMO4已知人肝脏mRNA按照FMO3≥ FMO5≥FMO4的顺序编码FMOs, FMO4的浓度和活性均很低, 并非肝脏中参与药物代谢的主要酶。人FMO4的突变型是所有FMOs中最为复杂的同工酶, 目前已鉴定出全长以及突变型的FMO4, 全长型FMO4主要存于肝脏和肾脏, 脑中也有少量存在[22]。
4.3.5 FMO5FMO5在成人肝脏、小肠、肾、肺等组织中表达较高, 占肝脏中总FMOs的50%, 很少发现其突变型。虽然FMO5能催化某些短链脂肪胺如N-辛胺的N-氧化以及某些含硫物如杀虫剂倍硫磷、抗风湿药艾那莫德的S-氧化, 但因其具有相对于FMO1或FMO3更深的底物结合区, FMO5很少参与FMOs特征底物如苄达明、三甲胺的氧化反应[65], 因此长期以来FMO5在药物代谢方面的作用常被忽视。近期研究发现, FMO5不仅能参与食物来源的脂肪酮(如庚酮)、环酮类(如薄荷酮)以及醛类(如茴香醛)等的氧化, 还能催化抗癌药物ER-879819和抗菌药MRX-1314生成酯[66], 因此上述化合物可以作为测定FMO5活性的探针底物。此外, 通过小鼠FMO5基因敲除表明, FMO5也参与内源性物质的代谢, 通过下调与糖脂代谢相关的催化酶等多重作用促进代谢老化[67]。
应当指出的是, FMOs的个体间差异多由于基因突变, 但FMO5的突变多由生理因素或者化学物质诱导, 如合成孕激素R5020、利福平、管叶金丝桃素分别增加乳腺癌细胞、人肝细胞、和HepG2中的FMO5基因表达水平[68]。
5 FMOs与CYPs鉴定的区别在以往的研究中, 通常认为CYPs是参与药物和外源物代谢的主要Ⅰ相代谢酶。因FMOs与CYPs具有相似的分子质量、底物特异性、组织和细胞分布以及实验条件的影响因素, 微粒体FMOs对药物代谢的贡献常被低估。随着越来越多的FMOs底物被发现, FMOs与CYPs在药物代谢方面的差异也逐渐得到重视。
首先, FMOs与CYPs的催化机制具有明显区别。其次, 在底物选择性方面, FMOs倾向于催化亲核化合物的氧化, 而CYPs则更易氧化低亲核化合物。虽然FMOs与CYPs都能催化含氮、硫的杂原子氧化, 但CYPs多催化碳原子的羟基化、脱烷基化以及环氧化, 易生成活性及潜在毒性的代谢产物, 部分产物还可抑制CYPs的活性。相反, FMOs是通过双电子机制催化亲核杂原子化合物氧化, 通常生成极性、易排出体外的低毒产物, 且产物不会抑制FMOs的活性。CYPs通常依靠转录调控表达水平, 但目前并没有通过转录来调控FMOs表达的相关报道。同时, 也没有报道证明转录后翻译对FMO的表达有明显的作用[69]。
通常区分这两种酶的方法是热灭活FMOs和用抑制剂抑制CYPs活性。在不存在NADPH的条件下, FMOs在55 ℃条件下不稳定, 而相同条件下CYPs能保持80%以上的活性, 因此可以在不加入NADPH时通过55 ℃预温孵来抑制FMOs的活性。另一区分FMOs与CYPs的方法是加入CYPs抑制剂如N-苄基咪唑或去污剂, 可明显抑制CYPs活性而基本不影响FMOs活性。但一些CYPs的抑制剂如SKF525A是FMOs的底物, 因此可能会通过底物选择性竞争而抑制FMOs。此外, FMOs与CYPs的最适pH值不同, FMOs为pH 9~10, CYPs为pH 7.4, 因此可在pH 8.4~9.4的条件下预温孵肝微粒体以抑制CYPs的活性[70]。目前可通过重组酶准确鉴定FMOs是否参与某一化合物的代谢。
6 FMOs介导的药物相互作用在新药研发的过程中, 寻找由非CYP酶参与代谢的候选化合物来降低由代谢酶介导的药物相互作用是近年来新药筛选的新方向。例如, 西沙必利与伊托必利是用于治疗胃食管反流的促动力药物, 西沙必利在体内由CYP3A4代谢脱烷基, 当与其他药物合用时会因为对CYP3A4的抑制作用从而使西沙必利的血药浓度升高, 引起QT间期延长并伴有室性心律不齐的风险; 而依托比利不经过CYP3A4代谢且只由FMO3代谢生成N-氧化产物。由于FMO3不易被诱导或抑制, 使用伊托必利代替西沙必利可降低药物-药物相互作用的风险[25]。又如抗精神病药奥氮平由CYP1A2、CYP2D6和FMO3参与代谢, CYP2D6和FMO3虽然存在个体间基因差异, 但并不能引起奥氮平体内外代谢的差异, 因此推测由多酶参与的代谢, 可以通过代偿作用降低药物的相互作用[71]。
Shimizu等[72]鉴定了41种含N/S的化合物对FMO3参与的苄达明N-氧化的抑制作用, 结果表明三甲胺、甲硫咪唑、伊托必利、陶扎色替可抑制约50%苄达明N-氧化, 随后证实甲硫咪唑也能抑制硫化舒林酸的S-氧化, 其他含N/S化合物对FMO活性影响较小, 不仅说明FMOs不易被诱导或者抑制, 也提示由FMOs参与代谢的N/S化合物间的相互作用较小, 可为类似结构的候选药物设计提供依据。苄达明的N-氧化和硫化舒林酸的S-氧化可作为FMO3参与的药物相互作用研究的探针底物。
7 FMOs与临床疾病7.1 三甲胺尿症FMO3的无功能突变会导致遗传性疾病, 如三甲胺尿症。三甲胺(trimethylamine, TMA)是一种有鱼腥味的气体, 通过肠道菌群分解饮食中的胆碱或者肉毒碱而生成三甲胺并吸收进入血液循环, 被FMO3氧化成氮氧化物(TMAO)排出体外。基因变异可造成FMO3功能缺失, 使TMA不能氧化成TMAO, 从而使高浓度三甲胺通过尿液和汗液排除体外, 使患者散发出鱼腥味, 因此也叫做鱼腥综合征[73]。除基因突变外, 人性激素、FMO3抑制剂或肝脏、肾脏疾病等因素使FMO3活性降低时也会导致TMAO/TMA比例上升, 出现三甲胺尿症的症状及对某些药物代谢能力的改变。
7.2 糖脂代谢和动脉粥样硬化FMO3在糖尿病中作用的早期研究主要集中在啮齿类动物模型, 发现FMO3缺陷可导致循环系统和肝脏中糖脂水平的下降, 相反FMO3过表达可提高糖脂水平, 推测体内FMO3是通过PPARα和Kruppel-样因子15 (KLF15) 途径调节糖脂水平, 而非直接通过TMA或者TMAO途径[74]。预测降低FMOs活性至正常水平之下可预防糖尿病引发的动脉粥样硬化。
7.3 帕金森症近年来发现脑中FMOs也具有一定的功能。在神经毒素鱼藤酮(rotenone)诱发的帕金森模型中, 通过FMOs抑制剂甲硫咪唑抑制FMOs活性, 能直接引起半胱天冬酶3 (活化的半胱天冬酶3可诱发细胞凋亡)活性增强, 同时引起Parkin蛋白(可维持多巴胺能神经元的正常功能)表达下降。因此推测, FMOs功能紊乱是鱼藤酮诱导帕金森模型中多巴胺能细胞凋亡的一个原因, 为病理模型研究提供了一个新的线索[75]。
8 总结与展望FMOs能催化多种药物、饮食成分以及杀虫剂等外源物的氧化, 生成极性大、易排出体外的代谢产物, 该酶的底物广泛性与其独特的催化机制相关。FMOs不易被诱导或者抑制, 表达水平存在明显组织、年龄、性别以及种属差异, 且存在多种基因突变, 引起酶数量和活性改变, 从而影响药物的疗效。近年发现FMOs与多种疾病的发生发展相关, FMO3的无功能突变不仅可引起三甲胺尿症, 也与体内糖脂水平下降有关。此外, FMOs功能紊乱者可能有帕金森症和脑卒中的风险。
虽然以往的观点认为FMOs在药物代谢中发挥的作用很小, 但FMOs参与药物代谢的优势日益受到重视。未来FMOs基因表型研究可作为预测药物代谢的个体差异一种手段, 有助于为新药的临床合理应用提供参考。另一方面, 基于大多数药物不是FMOs的底物, 引起对FMOs选择性抑制的可能较小, 且FMOs不易被诱导或抑制, 设计由FMOs参与代谢的新候选药物可能降低药物相互作用的风险。此外, FMOs功能研究为病理模型研究提供了新线索, 并可考虑以FMOs为靶点设计具有新作用机制的药物。
| [1] | Krueger SK, Williams DE. Mammalian flavin-containing monooxygenases: structure/function, genetic polymorphisms and role in drug metabolism[J]. Pharmacol Ther, 2005, 106: 357–387. DOI:10.1016/j.pharmthera.2005.01.001 |
| [2] | Fiorentini F, Geier M, Binda C, et al. Biocatalytic charac terization of human FMO5: unearthing Baeyer-Villiger reac tions in humans[J]. ACS Chem Biol, 2016, 11: 1039–1048. DOI:10.1021/acschembio.5b01016 |
| [3] | Fan PW, Zhang D, Halladay JS, et al. Going beyond common drug metabolizing enzymes: case studies of biotransformation involving aldehyde oxidase, γ-glutamyl transpeptidase, cathepsin b, flavin-containing monooxygenase, and ADP-ribosyltrans ferase[J]. Drug metab Dispos, 2016, 44: 1253–1261. DOI:10.1124/dmd.116.070169 |
| [4] | Ziegler DM, Mitchell CH. Microsomal oxidase. Ⅳ. Proper ties of a mixed-function amine oxidase isolated from pig liver microsomes[J]. Arch Biochem Biophys, 1972, 150: 116–125. DOI:10.1016/0003-9861(72)90017-3 |
| [5] | Tynes RE, Sabourin PJ, Hodgson E. Identification of distinct hepatic and pulmonary forms of microsomal flavin-containing monooxygenase in the mouse and rabbit[J]. Biochem Bio phys Res Commun, 1985, 126: 1069–1075. DOI:10.1016/0006-291X(85)90294-3 |
| [6] | Tynes RE, Hodgson E. Catalytic activity and substrate speci ficity of the flavin-containing monooxygenase in microsomal systems: characterization of the hepatic, pulmonary and renal enzymes of the mouse, rabbit, and rat[J]. Arch Biochem Biophys, 1985, 240: 77–93. DOI:10.1016/0003-9861(85)90010-4 |
| [7] | Atta-Asafo-Adjei E, Lawton MP, Philpot RM. Cloning, sequencing, distribution, and expression in Escherichia coli of flavin-containing monooxygenase 1C1. Evidence for a third gene subfamily in rabbits[J]. J Biol Chem, 1993, 268: 9681–9689. |
| [8] | Lang DH, Yeung CK, Peter RM, et al. Isoform specificity of trimethylamine N-oxygenation by human flavin-containing monooxygenase (FMO) and P450 enzymes: selective catalysis by FMO3[J]. Biochem Pharmacol, 1998, 56: 1005–1012. DOI:10.1016/S0006-2952(98)00218-4 |
| [9] | Chen Y, Zane NR, Thakker DR, et al. Quantification of flavin-containing monooxygenases 1, 3, and 5 in human liver microsomes by UPLC-MRM-based targeted quantitative proteomics and its application to the study of ontogeny[J]. Drug metab Dispos, 2016, 44: 975–983. DOI:10.1124/dmd.115.067538 |
| [10] | Taniguchi-Takizawa T, Shimizu M, Kume T, et al. Benzyda mine N-oxygenation as an index for flavin-containing monooxygenase activity and benzydamine N-demethylation by cytochrome P450 enzymes in liver microsomes from rats, dogs, monkeys, and humans[J]. Drug metab Pharmacokinet, 2015, 30: 64–69. DOI:10.1016/j.dmpk.2014.09.006 |
| [11] | Phillips IR, Shephard EA. Flavin-containing monooxy genases: mutations, disease and drug response[J]. Trends Pharmacol Sci, 2008, 29: 294–301. DOI:10.1016/j.tips.2008.03.004 |
| [12] | Kim YM, Ziegler DM. Size limits of thiocarbamides accepted as substrates by human flavin-containing monooxy genase 1[J]. Drug metab Dispos, 2000, 28: 1003–1006. |
| [13] | Korsmeyer KK, Guan S, Yang ZC, et al. N-Glycosylation of pig flavin-containing monooxygenase form 1: determination of the site of protein modification by mass spectrometry[J]. Chem Res Toxicol, 1998, 11: 1145–1153. DOI:10.1021/tx980117p |
| [14] | Siddens LK, Henderson MC, Vandyke JE, et al. Characteri zation of mouse flavin-containing monooxygenase transcript levels in lung and liver, and activity of expressed isoforms[J]. Biochem Pharmacol, 2008, 75: 570–579. DOI:10.1016/j.bcp.2007.09.006 |
| [15] | Hernandez D, Janmohamed A, Chandan P, et al. Organization and evolution of the flavin-containing monooxygenase genes of human and mouse: identification of novel gene and pseu dogene clusters[J]. Pharmacogenetics, 2004, 14: 117–130. DOI:10.1097/00008571-200402000-00006 |
| [16] | Dolphin CT, Cullingford TE, Shephard EA, et al. Differential developmental and tissue-specific regulation of expression of the genes encoding three members of the flavin-containing monooxygenase family of man, FMO1, FMO3 and FM04[J]. Eur J Biochem, 1996, 235: 683–689. DOI:10.1111/ejb.1996.235.issue-3 |
| [17] | Cherrington NJ, Ca oY, Cherrington JW, et al. Physiological factors affecting protein expression of flavin-containing monooxygenases 1, 3 and 5[J]. Xenobiotica, 1998, 28: 673–682. DOI:10.1080/004982598239254 |
| [18] | Uno Y, Shimizu M, Yamazaki H. Molecular and functional characterization of flavin-containing monooxygenases in Cynomolgus macaque[J]. Biochem Pharmacol, 2013, 85: 1837–1847. DOI:10.1016/j.bcp.2013.04.012 |
| [19] | Larsen-Su S, Krueger SK, Yueh MF, et al. Flavin-containing monooxygenase isoform 2: developmental expression in fetal and neonatal rabbit lung[J]. J Biochem Mol Toxicol, 1999, 13: 187–193. DOI:10.1002/(ISSN)1099-0461 |
| [20] | Cashman JR. Human flavin-containing monooxygenase: substrate specificity and role in drug metabolism[J]. Curr Drug metab, 2000, 1: 181–191. DOI:10.2174/1389200003339135 |
| [21] | Ziegler DM. An overview of the mechanism, substrate speci ficities, and structure of FMOs[J]. Drug metab Rev, 2002, 34: 503–511. DOI:10.1081/DMR-120005650 |
| [22] | Phillips IR, Dolphin CT, Clair P, et al. The molecular biology of the flavin-containing monooxygenases of man[J]. Chem Biol Interact, 1995, 96: 17–32. DOI:10.1016/0009-2797(94)03580-2 |
| [23] | Lin J, Cashman JR. Detoxication of tyramine by the flavin-containing monooxygenase: stereoselective formation of the trans oxime[J]. Chem Res Toxicol, 1997, 10: 842–852. DOI:10.1021/tx970030o |
| [24] | Lang DH, Rettie AE. In vitro evaluation of potential in vivo probes for human flavin-containing monooxygenase (FMO): metabolism of benzydamine and caffeine by FMO and P450 isoforms[J]. Br J Clin Pharmacol, 2000, 50: 311–314. |
| [25] | Furnes B, Schlenk D. evaluation of xenobiotic N-and S-oxidation by variant flavin-containing monooxygenase 1 (FMO1) enzymes[J]. Toxicol Sci, 2004, 78: 196–203. DOI:10.1093/toxsci/kfh079 |
| [26] | Yu J, Brown DG, Burdette D. In vitro metabolism studies of nomifensine monooxygenation pathways: metabolite identify cation, reaction phenotyping, and bioactivation mechanism[J]. Drug metab Dispos, 2010, 38: 1767–1778. DOI:10.1124/dmd.110.033910 |
| [27] | Kajita J, Inano K, Fuse E, et al. Effects of olopatadine, a new antiallergic agent, on human liver microsomal cytochrome P450 activities[J]. Drug metab Dispos, 2002, 30: 1504–1511. DOI:10.1124/dmd.30.12.1504 |
| [28] | Li F, Patterson AD, Krausz KW, et al. metabolomics reveals the metabolic map of procainamide in humans and mice[J]. Biochem Pharmacol, 2012, 83: 1435–1444. DOI:10.1016/j.bcp.2012.02.013 |
| [29] | Parte P, Kupfer D. Oxidation of tamoxifen by human flavin-containing monooxygenase (FMO) 1 and FMO3 to tamoxifen-N-oxide and its novel reduction back to tamoxifen by human cytochromes P450 and hemoglobin[J]. Drug metab Dispos, 2005, 33: 1446–1452. DOI:10.1124/dmd.104.000802 |
| [30] | Attar M, Dong D, Ling KH, et al. Cytochrome P450 2C8 and flavin containing monooxygenases are involved in the metabolism of tazarotenic acid in humans[J]. Drug metab Dispos, 2003, 31: 476–481. DOI:10.1124/dmd.31.4.476 |
| [31] | Yanni SB, Annaert PP, Augustijns P, et al. Role of flavin-containing monooxygenase in oxidative metabolism of voriconazole by human liver microsomes[J]. Drug metab Dispos, 2008, 36: 1119–1125. DOI:10.1124/dmd.107.019646 |
| [32] | Ring BJ, Wrighton SA, Aldridge SL, et al. Flavin-containing monooxygenase-mediated N-oxidation of the M1-muscarinic agonist xanomeline[J]. Drug metab Dispos, 1999, 27: 1099–1103. |
| [33] | Sz kő , Tábi T, Borbás T, et al. Assessment of the N-oxidation of deprenyl, methamphetamine, and amphetamine enantiomers by chiral capillary electrophoresis: an in vitro metabolism study[J]. Electrophoresis, 2004, 25: 2866–2875. DOI:10.1002/(ISSN)1522-2683 |
| [34] | Usmani KA, Chen WG, Sadeque AJM. Identification of human cytochrome P450 and flavin-containing monooxy genase enzymes involved in the metabolism of lorcaserin, a novel selective human 5-hydroxytryptamine 2C agonist[J]. Drug metab Dispos, 2012, 40: 761–771. DOI:10.1124/dmd.111.043414 |
| [35] | Potega A, Dabrowska E, Niemira M, et al. The imida zoacridinone antitumor drug, C-1311, is metabolized by flavin monooxygenases but not by cytochrome P450s[J]. Drug metab Dispos, 2011, 39: 1423–1432. DOI:10.1124/dmd.111.038984 |
| [36] | Joo J, Wu Z, Lee B, et al. In vitro metabolism of an estrogen-related receptor γ modulator, GSK5182, by human liver microsomes and recombinant cytochrome P450s[J]. Biopharm Drug Dispos, 2015, 36: 163–173. DOI:10.1002/bdd.v36.3 |
| [37] | Ballard JE, Prueksaritanont T, Tang C. Hepatic metabolism of MK-0457, a potent aurora kinase inhibitor: interspecies comparison and role of human cytochrome P450 and flavin-containing monooxygenase[J]. Drug metab Dispos, 2007, 35: 1447–1451. DOI:10.1124/dmd.107.015438 |
| [38] | Xie G, Wong CC, Cheng KW, et al. Regioselective oxidation of phospho-NSAIDs by human cytochrome P450 and flavin monooxygenase isoforms: implications for their pharmacoki netic properties and safety[J]. Br J Pharmacol, 2012, 167: 222–232. DOI:10.1111/j.1476-5381.2012.01982.x |
| [39] | Hamman MA, Haehner-Daniels BD, Wrighton SA, et al. Stereoselective sulfoxidation of sulindac sulfide by flavin-containing monooxygenases. Comparison of human liver and kidney microsomes and mammalian enzymes[J]. Biochem Pharmacol,, 2000, 60: 7–17. DOI:10.1016/S0006-2952(00)00301-4 |
| [40] | Hai X, Adams E, Hoogmartens J, et al. Enantioselective in-line and off-line CE methods for the kinetic study on cimetidine and its chiral metabolites with reference to flavin-containing monooxygenase genetic isoforms[J]. Electro phoresis, 2009, 30: 1248–1257. DOI:10.1002/elps.v30:7 |
| [41] | Francois AA, Nishida CR, Ortiz De Montellano PR, et al. Human flavin-containing monooxygenase 2.1 catalyzes oxygenation of the antitubercular drugs thiacetazone and ethionamide[J]. Drug metab Dispos, 2009, 37: 178–186. DOI:10.1124/dmd.108.024158 |
| [42] | Ring BJ, Catlow J, Lindsay TJ, et al. Identification of the human cytochromes P450 responsible for the in vitro formation of the major oxidative metabolites of the antipsychotic agent olanzapine[J]. J Pharmacol Exper Ther, 1996, 276: 658–666. |
| [43] | Mayatepek E, Flock B, Zschocke J. Benzydamine metabo lism in vivo is impaired in patients with deficiency of flavin-containing monooxygenase 3[J]. Pharmacogenetics, 2004, 14: 775–777. DOI:10.1097/00008571-200411000-00009 |
| [44] | Tugnait M, Hawes EM, McKay G, et al. N-oxygenation of clozapine by flavin-containing monooxygenase[J]. Drug metab Dispos, 1997, 25: 524–527. |
| [45] | Cashman JR, Xiong YN, Xu L, et al. N-Oxygenation of amphetamine and methamphetamine by the human flavin-containing monooxygenase (form 3): role in bioactivation and detoxication[J]. J Pharmacol Exp Ther, 1999, 288: 1251–1260. |
| [46] | Wang L, Christopher LJ, Cui D, et al. Identification of the human enzymes involved in the oxidative metabolism of dasatinib: an effective approach for determining metabolite formation kinetics[J]. Drug metab Dispos, 2008, 36: 1828–1839. DOI:10.1124/dmd.107.020255 |
| [47] | Luo JP, Vashishtha SC, Hawes EM, et al. In vitro identifica tion of the human cytochrome p450 enzymes involved in the oxidative metabolism of loxapine[J]. Biopharm Drug Dispos, 2011, 32: 398–407. DOI:10.1002/bdd.v32.7 |
| [48] | Lomri N, Yang Z, Cashman JR. expression in Escherichia coli of the flavin-containing monooxygenase D (form Ⅱ) from adult human liver: determination of a distinct tertiary amine substrate specificity[J]. Chem Res Toxicol, 1993, 6: 425–429. DOI:10.1021/tx00034a006 |
| [49] | Kousba A, Soll R, Yee S, et al. Cyclic conversion of the novel Src kinase inhibitor[J]. Drug metab Dispos, 2007, 35: 2242–2251. DOI:10.1124/dmd.107.017384 |
| [50] | Jacobsen W, Christians U, Benet LZ. In vitro evaluation of the disposition of a novel cysteine protease inhibitor[J]. Drug metab Dispos, 2000, 28: 1343–1351. |
| [51] | Prueksaritanont T, Lu P, Gorham L, et al. Interspecies comparison and role of human cytochrome P450 and flavin-containing monooxygenase in hepatic metabolism of L-775, 606, a potent 5-HT (1D) receptor agonist[J]. Drug metab Dispos, 2000, 30: 47–59. |
| [52] | Rawden HC, Kokwaro GO, Ward SA, et al. Relative contri bution of cytochromes P-450 and flavin-containing monoxy genases to the metabolism of albendazole by human liver microsomes[J]. Br J Clin Pharmacol, 2000, 49: 313–322. |
| [53] | Ohmi N, Yoshida H, Endo H, et al. S-Oxidation of S-methyl-esonarimod by flavin-containing monooxygenases in human liver microsomes[J]. Xenobiotica, 2003, 33: 1221–1231. DOI:10.1080/00498250310001624627 |
| [54] | Meng J, Zhong D, Li L, et al. metabolism of MRX-Ⅰ, a novel antibacterial oxazolidinone, in humans: the oxidative ring opening of 2, 3-dihydropyridin-4-one catalyzed by non-P450 enzymes[J]. Drug metab Dispos, 2015, 43: 646–659. DOI:10.1124/dmd.114.061747 |
| [55] | Yamazaki M, Shimizu M, Uno Y, et al. Drug oxygenation activities mediated by liver microsomal flavin-containing monooxygenases 1 and 3 in humans, monkeys, rats, and minipigs[J]. Biochem Pharmacol, 2014, 90: 159–165. DOI:10.1016/j.bcp.2014.04.019 |
| [56] | Burnett VL, Lawton MP, Philpot RM. Cloning and sequencing of flavin-containing monooxygenases FMO3 and FMO4 from rabbit and characterization of FMO3[J]. J Biol Chem, 1994, 269: 14314–14322. |
| [57] | Koukouritaki SB, Simpson P, Yeung CK, et al. Human hepatic flavin-containing monooxygenases 1 (FMO1) and 3 (FMO3) developmental expression[J]. Pediatr Res, 2002, 51: 236–243. DOI:10.1203/00006450-200202000-00018 |
| [58] | Ruffatti A, Del Ross T, Ciprian M, et al. Risk factors for a first thrombotic event in antiphospholipid antibody carriers: a prospective multicentre follow-up study[J]. Ann Rheum Dis, 2011, 70: 1083–1086. DOI:10.1136/ard.2010.142042 |
| [59] | Dolphin CT, Beckett DJ, Janmohamed A, et al. The flavin-containing monooxygenase 2 gene (FMO2) of humans, but not of other primates, encodes a truncated, nonfunctional protein[J]. J Biol Chem, 1998, 273: 30599–30607. DOI:10.1074/jbc.273.46.30599 |
| [60] | Krieter PA, Ziegler DM, Hill KE, et al. Increased biliary GSSG efflux from rat livers perfused with thiocarbamide substrates for the flavin-containing monooxygenase[J]. Mol Pharmacol, 1984, 26: 122–127. |
| [61] | Park CS, Kang JH, Chung WG, et al. Ethnic differences in allelic frequency of two flavin-containing monooxygenase 3 (FMO3) polymorphisms: linkage and effects on in vivo and in vitro FMO activities[J]. Pharmacogenetics, 2002, 12: 77–80. DOI:10.1097/00008571-200201000-00011 |
| [62] | Catucci G, Occhipinti A, Maffei M, et al. Effect of human flavin-containing monooxygenase 3 polymorphism on the metabolism of aurora kinase inhibitors[J]. Int J Mol Sci, 2013, 14: 2707–2716. DOI:10.3390/ijms14022707 |
| [63] | Kang JH, Chung WG, Lee KH, et al. Phenotypes of flavin-containing monooxygenase activity determined by ranitidine N-oxidation are positively correlated with genotypes of linked FM03 gene mutations in a Korean population[J]. Pharmacogenetics, 2000, 10: 67–78. DOI:10.1097/00008571-200002000-00009 |
| [64] | Cashman JR, Zhang J. Human flavin-containing monooxy genases[J]. Annu Rev Pharmacol Toxicol, 2006, 46: 65–100. DOI:10.1146/annurev.pharmtox.46.120604.141043 |
| [65] | Cashman JR. Role of flavin-containing monooxygenase in drug development[J]. Expert Opin Drug metab Toxicol, 2008, 4: 1507–1521. DOI:10.1517/17425250802522188 |
| [66] | Lai WG, Farah N, Moniz GA, et al. A Baeyer-Villiger oxidation specifically catalyzed by human flavin-containing monooxygenase 5[J]. Drug metab Dispos, 2011, 39: 61–70. DOI:10.1124/dmd.110.035360 |
| [67] | Gonzalez Malagon SG, Melidoni AN, Hernandez D, et al. The phenotype of a knockout mouse identifies flavin-containing monooxygenase 5 (FMO5) as a regulator of metabolic ageing[J]. Biochem Pharmacol, 2015, 96: 267–277. DOI:10.1016/j.bcp.2015.05.013 |
| [68] | Miller MM, James RA, Richer JK, et al. Progesterone regulated expression of flavin-containing monooxygenase 5 by the B-isoform of progesterone receptors: implications for tamoxifen carcinogenicity[J]. J Clin Endocrinol metab, 1997, 82: 2956–2961. DOI:10.1210/jcem.82.9.4239 |
| [69] | Cashman JR. Some distinctions between flavin-containing and cytochrome P450 monooxygenases[J]. Biochem Biophys Res Commun, 2005, 338: 599–604. DOI:10.1016/j.bbrc.2005.08.009 |
| [70] | Grothusen A, Hardt J, Br utigam L, et al. Convenient method to discriminate between cytochrome P450 enzymes and flavin-containing monooxygenases in human liver microsomes[J]. Arch Toxicol, 1996, 6: 64–71. |
| [71] | Okubo M, Narita M, Murayama N, et al. Individual diffe rences in in vitro and in vivo metabolic clearances of the antipsychotic drug olanzapine from non-smoking and smoking Japanese subjects genotyped for cytochrome P4502D6 and flavin containing monooxygenase 3[J]. Hum Psychopharmacol, 2016, 31: 83–92. DOI:10.1002/hup.v31.2 |
| [72] | Shimizu M, Shiraishi A, Sato A, et al. Potential for drug interactions mediated by polymorphic flavin-containing monooxygenase 3 in human livers[J]. Drug metab Pharma cokinet, 2015, 30: 70–74. DOI:10.1016/j.dmpk.2014.09.008 |
| [73] | Dolphin CT, Riley JH, Smith RL, et al. Structural organiza tion of the human flavin-containing monooxygenase 3 gene (FMO3), the favored candidate for fish-odor syndrome, deter mined directly from genomic DNA[J]. Genomics, 1997, 46: 260–267. DOI:10.1006/geno.1997.5031 |
| [74] | Shih DM, Wang Z, Lee R, et al. Flavin containing monooxy genase 3 exerts broad effects on glucose and lipid metabolism and atherosclerosis[J]. J Lipid Res, 2015, 56: 22–37. DOI:10.1194/jlr.M051680 |
| [75] | Li B, Yuan Y, Zhang W, et al. Flavin-containing monooxy genase, a new clue of pathological proteins in the rotenone model of parkinsonism[J]. Neurosci Lett, 2014, 566: 11–16. DOI:10.1016/j.neulet.2013.11.036 |